The Science Behind The Menopause Belly: And What Actually Works To Address It

Share
Here’s what I hear in my practice almost daily:
“I’m doing everything the same as I always have, but the weight just keeps piling on around my middle. My jeans don’t fit. I look down and see this belly that wasn’t there before. What’s wrong with me?”
I know this frustration personally. During my own perimenopause, I watched my body change in ways that felt completely foreign. Despite maintaining the same eating habits and exercise routine that had always worked, I developed what felt like a completely different midsection. My patients describe it the same way: “It’s like someone inflated a balloon in my stomach overnight.”
The answer? Nothing is wrong with you.
Like it or not, your body is responding predictably to the hormonal changes of perimenopause and menopause. The “menopause belly” isn’t a moral failing, it’s biochemistry.
What Exactly Is the Menopause Belly?
The menopause belly isn’t just “weight gain.” It’s a specific, predictable pattern of body composition change that affects nearly every woman during the hormonal transition of menopause.
As estrogen levels decline, women lose muscle mass while gaining fat mass, and that fat tends to accumulate around the abdomen rather than the hips and thighs. This is a biological shift from a “pear” to an “apple” shape, driven by changes in reproductive hormones.
Two types of abdominal fat contribute to this change:
Subcutaneous fat: The pinchable fat under the skin, aka the “muffin top.” It is usually more equally distributed and may be adapted through lifestyle modifications.
Visceral fat: The deeper fat surrounding internal organs like the liver and intestines. This fat creates that firm, distended feeling many women describe as a “hard belly.” It lies deep in the abdominal cavity, surrounding vital organs including the liver, stomach, and intestines.

While subcutaneous fat is more of a cosmetic concern, visceral fat is metabolically active and inflammatory, increasing risk for heart disease, insulin resistance, and certain cancers. In essence, visceral fat turns the abdomen into an inflammatory organ which is why it matters so much for long-term health.
Why These Changes Happen: The Hormonal Roadmap
Menopause triggers a cascade of hormonal shifts that directly affect metabolism, fat distribution, and muscle maintenance. Here’s what’s happening inside your body:
Estrogen Decline
Estrogen helps regulate where fat is stored. When levels fall, fat storage shifts from hips and thighs to the abdomen.1
Relative Rise in Testosterone
When estrogen levels drop, the amount of available testosterone increases, triggering a redistribution of body fat to the abdominal region.2
Changes in Hunger Hormones
Declining estrogen reduces leptin (the hormone that tells you you’re full) and, when sleep is disrupted, increases ghrelin (the hunger hormone).2 This combination can lead to increased appetite and slower metabolism.
Loss of Muscle Mass
During menopause, lean muscle mass naturally declines, often by 5 to 10% per decade after age 50. Less muscle means a slower resting metabolism and more difficulty maintaining weight, even if eating habits stay the same.3
Inflammatory Shift in Fat Tissue
Fat cells themselves change in menopause, becoming larger and more inflamed. This promotes insulin resistance and makes a “calories in, calories out” approach far less effective.4
Your body isn’t broken. It’s following a predictable hormonal script.
The Inflammation Connection
Declining estrogen also contributes to higher inflammation levels throughout the body. This inflammation plays a key role not just in belly fat accumulation, but also in joint and muscle pain, brain fog, fatigue, and even mood changes.4
When fat tissue becomes inflamed, it further drives hormonal and metabolic imbalance creating a vicious cycle.4
What Actually Works: Evidence-Based Solutions
The key to addressing menopause-related body changes is to work with your body, not against it. Here’s what the science and clinical experience both confirm:
1. Resistance Training: The Non-Negotiable Foundation
Loss of muscle mass is one of the biggest drivers of metabolic slowdown. Resistance training (using weights, resistance bands, or bodyweight) is the single most effective way to reverse this process.
Benefits include:
- Reduced visceral and subcutaneous fat5
- Increased muscle strength and metabolism6
- Improved glucose control and inflammation markers7
Aim for 2 to 3 full body sessions per week using progressive overload, gradually increasing weight or resistance over time.5 Preserving and building muscle mass can profoundly affect not only your well-being and overall health but also your independence as you age.7
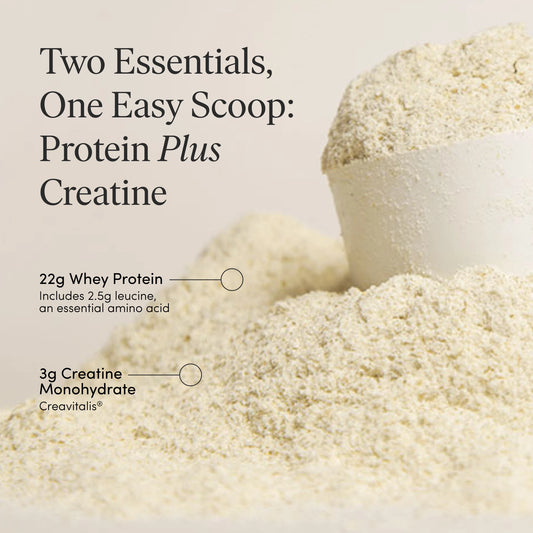
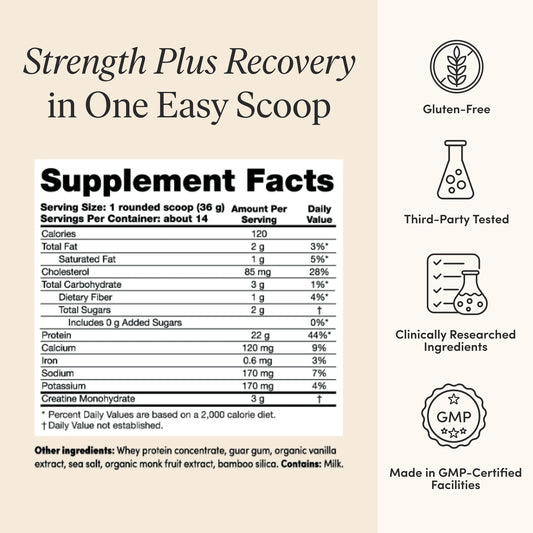
2. Eat More Protein (Seriously)
Your body’s protein needs rise during menopause. Higher protein intake helps preserve muscle, improve satiety, and maintain bone density.8
Aim for:
1.2–1.6 grams of protein per kilogram of body weight daily, spread evenly across meals (about 30g per meal for most women).8
Benefits include:
- Decreased muscle loss8
- Lower risk of frailty8
- Improved energy and mobility8
- Better weight maintenance8
Here’s an interesting fact. Increased protein intake and resistance training are the most prescribed non-pharmacological treatments used to maintain the health of aging populations.
3. Fiber: The Unsung Hero
Fiber supports your gut microbiome, improves insulin sensitivity, reduces inflammation, and helps manage appetite; all of which are critical during menopause.9
Work towards consuming 25 to 40 grams per day from whole, plant-based sources like berries, beans, whole grains, nuts, legumes, and vegetables with skin.10
If you struggle to meet this goal, consider supplementing with a high-quality soluble and insoluble fiber blend (like Fiber GDX) to support digestive regularity and keep you feeling great.
4. Reduce Added Sugar
Excess added sugar fuels inflammation and visceral fat storage. Keep intake below 25 grams of added sugar daily (this excludes naturally occurring sugars in fruit and dairy).11
Hidden sugars are common in salad dressings, sauces, and “low-fat” packaged foods. Reading labels and focusing on whole, unprocessed foods makes a huge difference.
5. Cardio in the “Fat-Burning Zone”
While resistance training builds muscle, Zone 2 cardio (low to moderate intensity) helps your body use fat for fuel.12
To determine your Zone 2 heart rate range, subtract your age from 220 to find your maximum heart rate (Mhr). Then, multiply your maximum heart rate by 0.60 and 0.70. This is your Zone 2 heart rate zone.
Alternatively, you can determine if you’re in Zone 2 by using the “talk test”. If you are slightly breathless but can maintain a conversation, you’re likely in Zone 2, hence the name "conversational cardio".
Walking, swimming, or cycling all work beautifully. Wearing a weighted vest during activity may also help you get into this heart rate zone.
6. Reduce Stress
Chronic stress raises cortisol, a hormone that increases belly fat storage and inflammation. It also worsens sleep, mood, and blood sugar control.
Incorporate daily stress management practices like:
- Journaling
- Meditation or prayer
- Restorative yoga or Tai Chi
- Breathing exercises
- Counseling or therapy
Even just five minutes of intentional calm can lower cortisol and reduce stress levels.13
7. Limit or Eliminate Alcohol
Alcohol can worsen hot flashes, disrupt sleep, elevate cortisol, and interfere with weight regulation. It also increases risk for bone loss and certain cancers. Taking a break, or better yet, avoiding alcohol completely can dramatically improve sleep, mood, and energy.14
8. Consider Hormone Therapy (HT)
Hormone therapy doesn’t cause weight gain, in fact, it can help reduce visceral fat accumulation and improve metabolic health.15 It may also improve sleep, mood, and energy, which indirectly support weight management.16, 17
Discuss with your healthcare provider whether HT is appropriate for you.
What Doesn’t Work
- Extreme calorie restriction: Slows metabolism and increases muscle loss.
- Cardio-only workouts: Don’t prevent muscle decline or improve metabolism.
- Generic “diet plans”: Ignore the hormonal context of menopause.
- Shame-based approaches: Increase cortisol and worsen fat storage.
A Comprehensive Approach
Women who succeed long-term use a whole-body strategy that includes:
- Resistance training 2 to 3 times per week
- Higher protein intake
- Plant-forward, high-fiber nutrition
- Regular Zone 2 cardio
- Stress and sleep optimization
- Consideration of HT when appropriate
- Supportive community and realistic expectations
This holistic approach addresses the root causes of menopause-related body composition changes rather than just symptoms.
The Mindset Shift That Changes Everything
The most powerful change isn’t physical: it’s mental.
Understanding that your body is following a biological blueprint, not “failing,” helps you approach your menopause with compassion and strategy instead of frustration. To avoid living the last third of our lives in poorer health, we must switch our focus and inner dialogue to strong over skinny and nutrition over calories.
Gone are the days of endless hours of cardio and calorie restriction. Instead, welcome the days of fueling your body with adequate nutrition, preserving and protecting your muscles and bones with resistance training, and moving your body to maintain and improve your cardiovascular health.
When you stop fighting your biology and start supporting it, your results and your confidence transform. What you do today will affect the woman you are in twenty or thirty years, so it’s time to get serious.
The Bottom Line
Your body isn’t broken. It’s responding exactly as it’s designed to during this transition.
Menopause-related weight changes are not inevitable, but they do require a different approach, one that honors your experience, supports your biology, rebuilds your muscle, and nourishes your metabolism from the inside out.
Work with your body, not against it and you’ll feel stronger, more balanced, and more in control than ever before.