The Metabolic Syndrome of Menopause: A New Framework for Midlife Health

Share
Let’s Rethink What Midlife Health Really Means
When we talk about menopause, most people think of hot flashes or mood swings. But there's a much deeper metabolic shift happening under the surface, one that directly impacts our heart, brain, and long-term health.
It’s called metabolic syndrome, and it’s one of the most overlooked health risks for women in midlife.
Even women who were totally healthy before menopause - a normal weight, good labs, active lifestyle - can suddenly find themselves gaining belly fat, watching their cholesterol rise, or developing high blood pressure for the first time.
This isn’t just anecdotal. In one large, multiethnic, long-term study, nearly 1 in 7 women developed metabolic syndrome by the time they reached their final menstrual period, even if they started out metabolically healthy.(1)
But here’s what really caught my attention: the risk of developing metabolic syndrome is actually higher during perimenopause than after menopause is complete.
Let me say that again. The time when most women are told, “You’re too young for hormones,” or “Let’s just wait and see,” is actually the most dangerous time to ignore what your body is telling you.
Why does this happen? Because your hormones are shifting dramatically, and those shifts can affect everything from how your body stores fat to how your cells use insulin to how your cholesterol behaves.
That’s why I call this the Metabolic Syndrome of Menopause. Because it’s not just about age or lifestyle. It’s about hormonal shifts that change the way your body works, from the inside out.
What Is the Metabolic Syndrome of Menopause?
This term refers to the cluster of physiological changes that occur as a direct result of declining estrogen and shifting hormones, which increases the risk of developing metabolic syndrome,(2) a group of conditions that includes:
- Central (abdominal) obesity
- Insulin resistance
- Dyslipidemia (high triglycerides and low HDL cholesterol)
- Elevated blood pressure
- Elevated fasting glucose
Having just three of these factors qualifies as metabolic syndrome, which is associated with higher risks of heart disease, stroke, type 2 diabetes, and even cognitive decline.(3)
During the menopause transition, studies have shown a marked increase in these risk factors, even when weight gain is modest or absent.(4) This is not about vanity or willpower. It’s biology.
Why Does Menopause Trigger Metabolic Syndrome?
We’ve often blamed the metabolic shifts of menopause on dropping estrogen levels, and that’s part of the story, but new research shows it’s not the whole picture.(5)
When estrogen declines, we see:
- More visceral fat around the belly, which is linked to inflammation and heart disease
- Decreased insulin sensitivity, making blood sugar harder to control
- Cholesterol changes, like rising triglycerides and lower HDL
- Higher blood pressure, due to stiffer blood vessels
- Muscle loss, which slows metabolism
These changes are compounded by age-related muscle loss (sarcopenia) and decreasing energy expenditure, creating a perfect storm for metabolic disruption.
Clinical Implications: This Isn’t Just About Weight Gain
Many women come to me frustrated by unexplained belly fat or fatigue. But what’s often missed by patients and doctors alike is that these symptoms are early signs of a metabolic shift with serious health consequences.(7)
Women in the menopause transition have an increased risk of:
- Cardiovascular disease (the #1 killer of women)
- Type 2 diabetes
- Cognitive decline and dementia
- Non-alcoholic fatty liver disease (NAFLD)
- Polycystic ovarian syndrome (PCOS) features re-emerging due to hyperinsulinemia
And yet, metabolic syndrome is underdiagnosed in women, especially during midlife, when the risk spikes the most.
How We Fight Back: A Midlife Health Framework
The good news? Midlife can be a time of powerful transformation. But we must be proactive.(8)
Here’s how I guide my patients through managing the metabolic syndrome of menopause:
1. Know Your Numbers, Because They Matter More Than the Scale
Let me be crystal clear: the scale alone does not tell the whole story of your health. In fact, many women look “healthy” on the outside but are silently developing insulin resistance, visceral fat accumulation, and inflammation on the inside.
This is why I’m such a big believer in knowing your metabolic numbers. These lab values and measurements can help uncover risks before they show up as disease. They can also give you the power to do something about it.
So here’s what I want you to ask your provider to check:
-
Body Composition Analysis: This is about more than vanity. It’s about visceral fat, the deep belly fat that wraps around your organs and drives inflammation and disease risk. DEXA scan or an electrical impedance monitor such as an InBody scale can provide critical body composition data. You can calculate your waist to hip ratio at home really easily using a soft tape measure as I demonstrate in this video. A measurement over 35 inches for women is considered a red flag.
-
HOMA Insulin Resistance Score: For this you need a fasting glucose and insulin: You need both. A normal fasting glucose can still hide insulin resistance. Elevated fasting insulin is often one of the first signs that your metabolism is struggling. Tools such as this online HOMA IR calculator can detect insulin resistance before the A1C rises.
-
Hemoglobin A1c: This shows your 3-month average blood sugar. Even values in the “normal” range (5.5–5.6%) can indicate prediabetes. Don’t wait until you cross the threshold! Catch it early.
-
Lipid panel: Ask for the full breakdown. That is total cholesterol, LDL, HDL, and triglycerides. Also ask for Apo B and Lp (a) which are more likely to be associated with the risk of cardiovascular disease. Estrogen loss shifts our lipids in the wrong direction, but we can intervene. Look especially at low HDL and high triglycerides, both of which increase with insulin resistance.
- Blood pressure: Menopause can bring subtle changes that nudge BP up over time. If your pressure starts creeping above 120/80, it’s a signal that your metabolic system may need attention.
These aren’t just numbers on a chart, they are windows into your future health.
You deserve to know where you stand. And if your provider dismisses your concerns or tells you “everything is normal” when your gut says something’s off, find one who will listen. We need to stop normalizing midlife decline and start getting proactive about prevention.
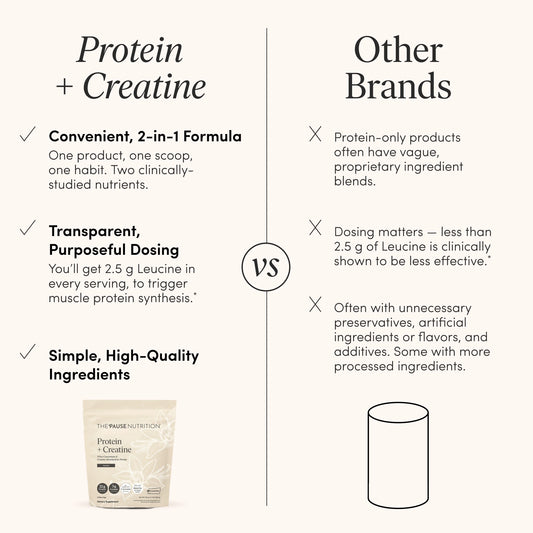
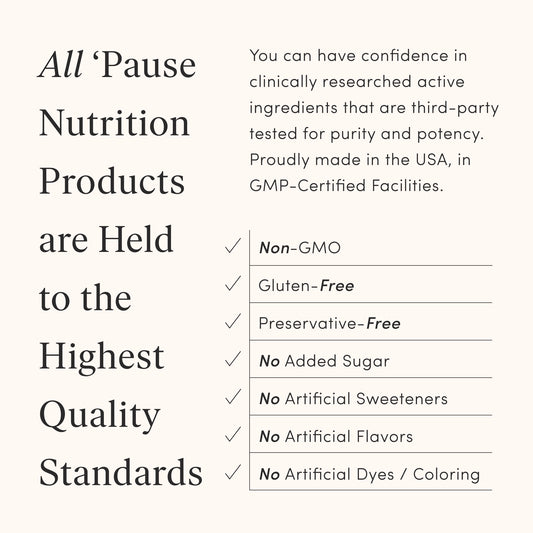
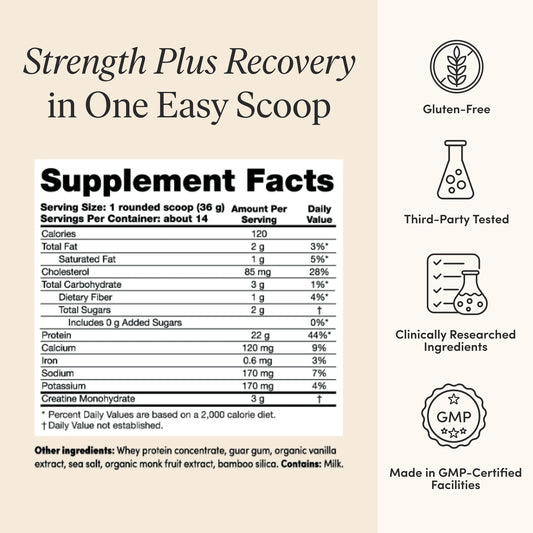
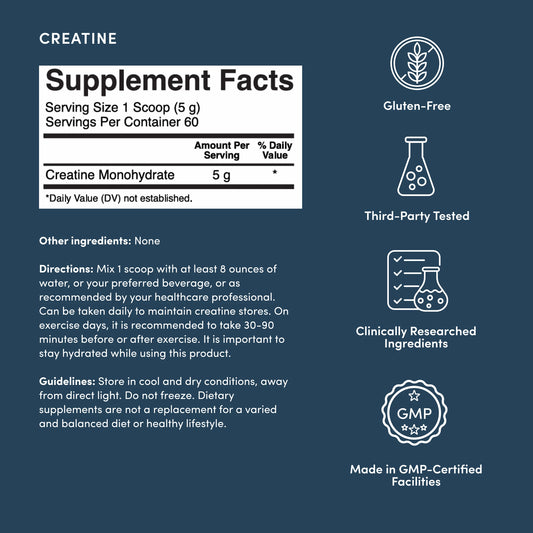
2. Prioritize Protein and Strength Training
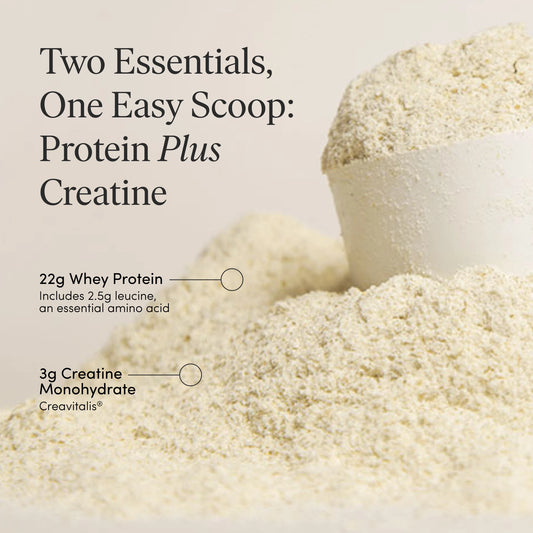
Muscle is metabolically protective. Aim for 1.5 to 1.8g of protein per kg of body weight and resistance training at least 2–3 times per week to combat sarcopenia and insulin resistance.
Use my protein calculator here to find your ideal protein range.
3. Reduce Added Sugars and Processed Carbs
Insulin resistance thrives on ultra-processed foods. Transition to a Mediterranean-style diet rich in fiber, omega-3s, and phytonutrients to stabilize blood sugar.
Learn more in The Belly Fat Blast Challenge.
4. Consider Hormone Replacement Therapy (HRT)
Evidence suggests that transdermal estrogen therapy started near menopause can help reduce visceral fat, improve lipid profiles, and preserve insulin sensitivity. It’s not just about symptom relief, it’s about disease prevention.
Always talk to your doctor about whether hormone therapy is right for you.
5. Support Sleep, Stress, and Recovery
Chronic stress increases cortisol, which worsens insulin resistance and contributes to weight gain, fatigue, and brain fog. That’s why prioritizing quality sleep and managing stress is absolutely essential in menopause. It is also why it can feel so frustrating when your sleep starts to fall apart, right when you need it most.
Here’s what I want you to know: declining hormones, especially progesterone, can play a major role in midlife insomnia.
Progesterone is your body’s natural calming hormone. It activates GABA receptors in the brain, which promote relaxation and deeper, more restorative sleep. When levels drop in perimenopause, it’s common to experience:
- Difficulty falling asleep
- Frequent nighttime waking
- Early morning awakenings
- Increased anxiety or restlessness at night
And here’s the kicker: many women are prescribed sleeping pills or anti-anxiety medications when hormone therapy (HT) may address the root cause.
💡 Micronized progesterone (often prescribed orally as Prometrium®) has been shown in studies to improve sleep onset and quality, especially when used alongside estrogen therapy. It mimics the body’s natural progesterone and can help restore hormonal balance without sedation or next-day grogginess.(9)
👉 Talk to your doctor before reaching for a prescription sleep aid or SSRI. Adding circadian rhythm support with Pause SleepTM and replacing the hormones your body is missing, particularly progesterone, might be the key to better sleep, calmer nights, and a clearer head during the day.* Tracking your sleep with a wearable device such as an Oura ring, can be extremely helpful as well.
And of course, layer in other supportive habits:
- Consistent sleep and wake times
- Mindfulness, breathwork, or yoga
- Limiting alcohol and blue light before bed
- Pay attention to your magnesium intake for relaxation support
6. Don’t Delay Treatment. If Your Doctor Recommends Medication, It’s for a Reason.
Let me say something loud and clear: needing medication does not mean you’ve failed. It means your body is sending a signal, and you’re choosing to listen.
Whether it’s a blood pressure med, a statin, metformin, or a GLP-1 medication, these are tools. Tools that can help you interrupt a dangerous metabolic spiral and protect your long-term health.
Too many women put off treatment because we’ve been taught to “just try harder,” to handle everything with willpower or a new exercise or diet trend. Don’t get me wrong, lifestyle matters, but sometimes, lifestyle alone isn’t enough, especially in the hormonal landscape of menopause.
Let’s look at GLP-1 medications, for example. These drugs mimic a hormone that helps regulate insulin, appetite, and body weight. And yes, they’re showing promise for women in menopause, who often struggle with stubborn fat gain, especially around the belly.
A new study looked at postmenopausal women taking semaglutide over 4 months.(10) Despite starting with higher weight and more fat mass, these women lost just as much weight and fat as their premenopausal counterparts. Crucially, they preserved lean muscle mass along the way.
This is a big deal. Because in menopause, we’re not just fighting weight gain, we’re fighting increased visceral fat, insulin resistance, and sarcopenia (muscle loss). A tool that can help reduce fat while preserving lean mass is worth serious consideration.
So if your provider says you’d benefit from starting a statin, or your blood pressure is creeping up, or they suggest a GLP-1 to support weight loss and metabolic control, don’t brush it off. These medications aren’t “giving up.” They’re giving your body a fighting chance.
The goal is not perfection. The goal is prevention.
Don’t wait until you’re in a crisis to take your health seriously. Be proactive. Ask questions. Advocate for care that reflects what we now know about how menopause changes our biology.
Bottom Line: You’re Not Broken, You’re Changing
The Metabolic Syndrome of Menopause is real, measurable, and treatable. Naming it gives us power. Addressing it gives us our health back.
So if you’re noticing changes in your body, energy, or labs, don’t ignore them. Talk to your provider. Ask the right questions. And advocate for the care that reflects the reality of midlife metabolism.
And if you want more tools to feel your strongest in midlife, join the Pause Strong Challenge.
This article contains affiliate links.