A Man’s Guide to Menopause: Understanding and Supporting Her Journey

Share
When women start to realize that their bodies are changing as menopause approaches, there can be a tendency to keep it to themselves. It can feel uncomfortable to tell a partner about thinning hair, painful sex or or feeling hot and sweaty all the time.
But these days, a growing number of men are starting the conversation. Loving and curious men are going to the doctor with their partners to learn and offer moral support. And fortunately, this seems to be a growing trend. In a 2019 survey of 450 men, 72 percent reported talking to their partners about menopause symptoms, while 75 percent believed they helped influence their partners to seek treatment or make lifestyle changes. As journalist Tamsen Fadal told USA Today, “Half of the population will go through menopause, and we need the other half to understand it.” At long last, it seems that men and male doctors are joining the larger conversation about how to support their wives, mothers, sisters and patients through the menopause transition.
That support comes in the form of funny posts like this one by urologist Hunter Norton, MD explaining how declining estrogen can make you feel like you have to “go” all the time and @popzthedancer talking about wearing a hat and coat inside the house because the thermostat is set so low. There’s the quiet outrage as Peter Attia, MD and Rachel Rubin, MD break down how the WHI study (which scared generations of women away from hormone therapy) turned out to be the biggest medical injustice in modern medicine, on the Drive podcast.
Even though men don’t experience hot flashes or many of the other symptoms associated with the menopause transition, they understand that menopause is happening to them too. They’re also realizing that they can play a role in making the transition easier for the women in their lives, and for themselves.
A few years ago, it would have been hard to imagine that some of the top male podcasters like Steven Bartlett of Diary of CEO or Andrew Huberman of The Huberman Lab, would spotlight menopause, however, by sharing their platforms, they’re helping get the menopause message out to millions of men.
Here’s what men need to know about perimenopause and menopause.
What is menopause?
Menopause is the one-year anniversary of a woman’s last period. This usually happens around age 51 or 52, but with some women it happens earlier. Menopause can start all of a sudden if a woman has a hysterectomy, other surgery to remove her ovaries or a health condition that requires treatment that affects the function of her ovaries.
The years leading up to this one-day anniversary event are called perimenopause, which means “around menopause.” The perimenopause phase can start seven to 10 years before actual menopause, so some women are in their late 30s when they begin to experience hormonal fluctuations. Perimenopause has been referred to as the zone of chaos because the levels of three key hormones are changing, causing many of the symptoms associated with menopause.
What are the hormonal changes happening to a woman during perimenopause and menopause?
Healthy women have a balance of three main hormones: estrogen, progesterone and testosterone. During perimenopause, a woman’s levels of three key hormones start to fluctuate wildly. It can rock a woman’s world, affecting every part of her brain and body..
Here’s what each hormone does:
Estrogen - Estrogen is so much more than a sex hormone that controls periods and is necessary for making babies. Women have estrogen receptors in every body system, including the immune system, skin, bladder, bones, muscles and brain and these body systems rely on estrogen to function properly. A powerful anti-inflammatory, estrogen keeps joints and tendons moving freely and arteries flexible, which lowers cardiovascular risk. It powers a woman's brain, helping with learning, thinking, moods and temperature control, and when women start making less estrogen, all sorts of menopausal symptoms develop.
Progesterone - This hormone is the yin to estrogen’s yang, keeping the nervous system calm and supporting good sleep. Without it, women can be tired at night, but too agitated and restless to really relax and fall asleep. It also has important functions in maintaining our moods.
Loss of progesterone after menopause is linked to increased levels of depression, anxiety and insomnia.
Testosterone - While women have lower levels compared to men, they have testosterone too. It is produced in their ovaries and adrenal glands and supports healthy muscles, strong bones, energy and libido. Testosterone declines steadily as women and men age, and the perimenopause zone of chaos can leave them feeling exhausted and completely uninterested in sex.
What are some of the symptoms that occur during menopause?
Every woman is unique, and so is her menopause experience. A 2025 study of women using a menopause app noted 45 different symptoms, but here’s a rundown on some of the most common and distressing menopause symptoms:
Hot flashes - The most talked-about menopause symptom is hot flashes which cause sweating and flushing. They’re part of a trio of vasomotor symptoms that also includes heart palpitations and night sweats that can occur out of seemingly nowhere and daytime activities and sleep.
Mood changes - It is not discussed as often as it should be, but 70 percent of women experience mood changes ranging from sadness to irritability over seemingly small things (like someone chewing loudly to rage. Outside of mood changes, many women find themselves getting better at setting boundaries. Lisa Mosconi, PhD writes in her book The Menopause Brain “They describe the ability to draw the line regarding others’ needs, finally able to pay attention to their own.” Once they’re past the first couple years of the menopause transition, Mosconi notes that women report feeling happier and having greater empathy and emotional control than before ever.
Musculoskeletal changes - Without the antiinflammatory power of estrogen, women start having a range of musculoskeletal changes including aches and pains in their joints and backs without any new injury. Frozen shoulder, which can make it impossible to lift her arm, is one of the most common. Women also start to lose bone density in their 40s, so they may get a surprise diagnosis of osteopenia by their mid or late 40s.
Insomnia - A 2023 study noted that nearly 52 percent of postmenopausal women struggle to get enough sleep. With lower progesterone levels, it becomes harder to relax and experience restorative, sound sleep. Night sweats often disrupt sleep and chronic insomnia leaves women feeling cranky the following day, raises levels of the stress hormone cortisol, and over time, increases the risks of cardiovascular disease.
Weight and body composition changes - Even women who are religious about healthy eating and exercising regularly can still experience weight and body composition changes, gaining five, or 10 extra pounds, sometimes more, during perimenopause. The rate of fat gain doubles during this transition, while women are also losing muscle. This perfect storm causes weight to accumulate in the midsection, in the form of visceral, or intra-abdominal fat.
Lower sex drive - Between mood changes, lack of sleep, achy joints and feeling hot all the time, it’s not surprising that women often aren’t in the mood for intimacy. Lower testosterone levels affect libido, and for some menopausal women vaginal dryness can make sex painful.
What are the best solutions to menopause symptoms?
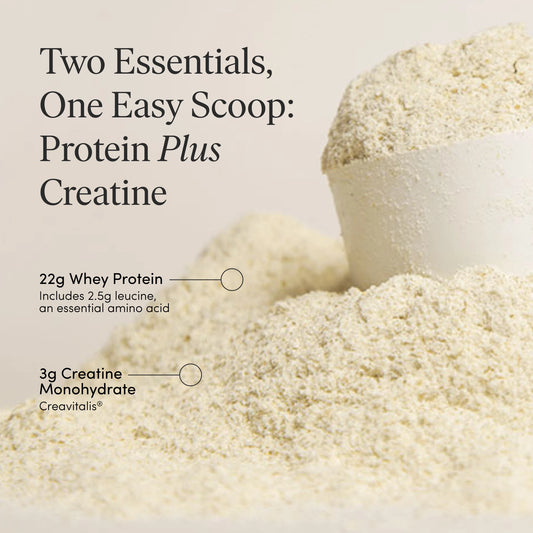
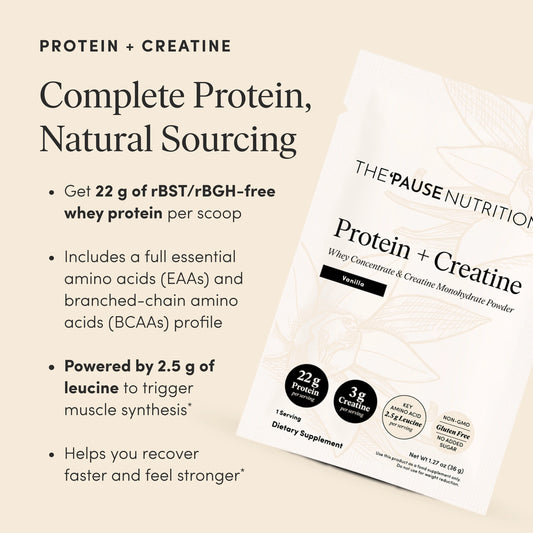
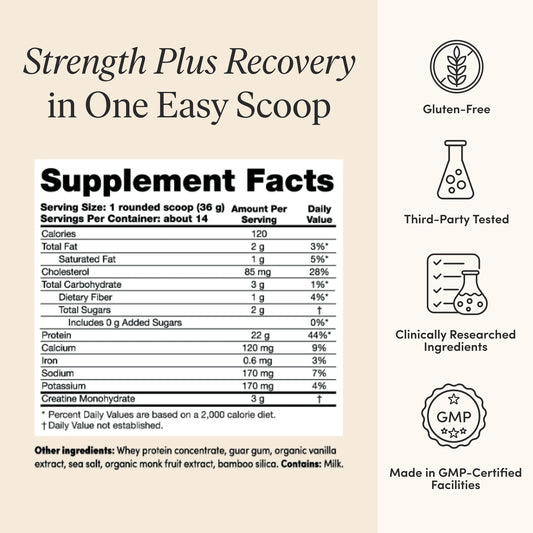
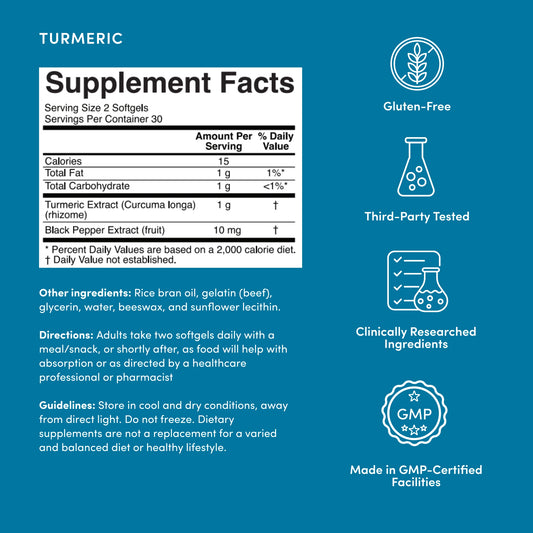
There are solutions to improve menopause symptoms that start with lifestyle choices that are all part of the Menopause Toolkit. Prioritizing protein and a fiber filled diverse anti-inflammatory diet, building muscle, managing stress and optimizing sleep can go a long way in improving quality of life.
When it comes to medical care, the most effective first-line treatment is bioidentical hormone therapy, which usually includes the estradiol form of estrogen and oral micronized progesterone. According to the Menopause Society’s latest guidelines, the benefits of hormone therapy outweigh the risks for most women, however many clinicians aren’t trained in menopause care and withhold hormone therapy, or send a woman home with an antidepressant. This is a massive injustice; a 2024 study that looked at healthcare costs for nearly 120,000 women with hot flashes noted that only 20 percent of them received treatment.
How can men help their partners through menopause?
If a woman in your life is discouraged and confused, doesn’t know where to turn for answers and solutions, or is not getting the necessary support from her doctor, don’t let her give up. Encourage her to seek help elsewhere. Help her find a new doctor, or suggest she consult a telemedicine company such as Midi Health, Alloy or Evernow. The ‘Pause Life website has a Clinicians List which is a compilation of practices that have been recommended by others who have had a positive experience, and may be a helpful resource. Every woman deserves a conversation with an informed clinician about the risks and benefits of hormone therapy.
You can help her prepare to talk to her clinician about hormone therapy, so she’s ready with a list of her symptoms and relevant studies. Or, work out with her so she can stay strong and healthy as she ages. Download the free Menopause Empowerment Guide, which includes helpful links and a plan for thriving during this transition. Deepen your understanding by reading books like The New Menopause, Estrogen Matters and others. Figure out what intimacy looks like for the two of you right now. Ask what kind of support she needs. Above all, believe her when she tells you what she’s feeling.
As the hilarious and insightful fitness coach Mitch Little puts it “Perimenopause and menopause isn’t a solo sport. It’s a team sport. So fellas, grab your partner by the hand, and support your partner through this time.”
The menopause transition brings challenges, but for couples and loved ones who are committed to tackling it together, it offers the opportunity for growth and creating an even stronger bond.
This article contains affiliate links.