Brain Fog - It's Not All In Your Head - How Does Menopause Affect the Brain?

Share
How Does Menopause Affect The Brain?
Many of the symptoms related to the menopause transition are easy to identify and communicate, such as weight gain, hot flashes and night sweats, but brain fog is different. The word itself feels fuzzy, and so does the experience.
That’s why many clinicians miss it or dismiss women’s concerns about changes in the way they’re thinking. Thanks to researchers like neuroscientist Dr. Lisa Mosconi, PhD, we know the brain undergoes striking structural and functional changes during menopause, more women are better equipped to communicate the changes they’re experiencing and more clinicians are listening.
What is Menopausal Brain Fog?
Brain fog is a catch-all term for a group of symptoms that can start in perimenopause, and sometimes last into post-menopause. Women who once felt unstoppable, running businesses, juggling family and multitasking with ease, feel overwhelmed and unable to keep up. The medical term for it is mental fatigue, and in many ways it can feel like your brain has run out of power. According to Mosconi’s book, The Menopause Brain, symptoms of brain fog may include:
- Forgetting names and events
- Losing keys, your phone, or your train of thought repeatedly
- Trouble concentrating
- New diagnosis of Attention Deficit Hyperactivity Disorder (ADHD)
- Slower comprehension or decision-making
- Struggling to multitask
- Feeling tired or sluggish
About 60% of women report memory problems during menopause.
How Menopause Changes the Brain
In a study of women in pre-, peri- and postmenopause, researchers used brain imaging to see how declining hormones affect the brain. They found mostly temporary changes in the parts of the brain responsible for cognition. Grey matter, the tissue that contains most of the brain’s nerve cells and is essential for thinking, memory, and decision-making, temporarily shrank, and the brain shifted its main fuel source, using less glucose and relying more on fat and ketones. Brain imaging also showed shifts in the areas that control movement, memory and emotions. The encouraging part is that after menopause the brain stabilized. Grey matter volume recovered, and the brain drew energy from another source. Mosconi says this suggests the brain is capable of compensating, adapting, and learning to work differently.
Researchers also found that during perimenopause, it can be harder to learn new information. This slower learning, along with misplaced keys and forgotten names, is usually temporary. As the brain remodels itself for this new stage of life, these changes tend to improve.
Does Brain Fog Cause Dementia or Alzheimer’s?
The short answer is no, but this concern is understandable. Women are twice as likely as men to develop Alzheimer’s over their lifetime, about 20% compared with 10%. Right now, women make up two-thirds of the 6.9 million Americans living with the disease. In the U.S., about 5% of females over age of 60, 12% after age 75, and 28% after age 85, have dementia.
For most women, though, that’s not the case. As Mosconi explains, the memory lapses and trouble learning improve after menopause. The Study of Women’s Health Across the Nation showed that women experienced a dip in cognitive test scores during perimenopause, that typically resolved by post-menopause.
There are exceptions. For women with a genetic predisposition, such as carrying the APOE-4 gene, lower levels of estrogen, the hormone that fuels and protects the brain, are linked to greater Alzheimer’s risk profiles and biomarker changes, according to Mosconi. Since only about 20% of women will ever develop dementia, researchers are now working to understand what raises or lowers each woman’s individual risk.
Mosconi’s 2021 study in Nature, found that women with the APOE-4 gene carry greater deposits of amyloid beta plaque in the brain, a marker for dementia. Research isn’t definitive on how hormone therapy affects dementia risk, but the findings are promising. A 2023 analysis of many studies concluded that when women begin hormone therapy early enough, it may help protect the brain from developing Alzheimer’s disease. Still, Mosconi says there isn't enough evidence to recommend hormone therapy as a prevention strategy for all women.
How Does Stress Affect the Brain During Menopause?
During menopause, the brain’s stress response shifts. With less estrogen there’s nothing to counterbalance the effect of stress hormones, especially cortisol, on the brain. That’s why many women feel more reactive, anxious, or mentally drained during this time. Interestingly, women on estradiol therapy report stress, but their cortisol levels are lower.
Estrogen and stress hormones have entirely opposite effects on the body. Estradiol supports brain health, while stress hormones work against it, interfering with our thinking and ability to respond to the environment, including how we remember, understand, learn, and process. Estradiol can help attenuate the negative effects of stress hormones on the brain.
Can Estrogen Therapy Help with Menopause Brain Fog?
Estradiol therapy may help decrease the body’s excess cortisol response to stress, preventing the adrenal glands from making more cortisol. Estradiol also protects the nerve cells in the brain from damaging chemicals, including cortisol.
One 2017 study of 42 menopausal women found that for those on long-term estradiol therapy, stress caused a smaller increase in cortisol, and it had less effect on their short-term memory. The women treated with estradiol had lower free cortisol levels than the placebo group, even when they were subjected to higher levels of stress.
While your doctor won’t prescribe estrogen therapy just to treat brain fog alone, it’s a potential side benefit to using hormone therapy to manage your hot flashes or risk of genitourinary issues.
But What if You Can’t, or Choose Not to, Take Estrogen?
Estrogen therapy isn’t an option for all women, and the decision to take hormone therapy must always be made in consultation with your doctor, based on your health history and risk profile. But there are still proven ways to support brain health during menopause.
Lifestyle choices play a powerful role. There is robust evidence that lifestyle habits, such as adequate sleep, regular exercise and anti-inflammatory nutrition, may help protect emotional balance and cognitive function.
When it comes to diet, Mosconi points to the Mediterranean diet as one of the best places to start. This style of eating is rich in leafy greens, colorful fruits, legumes, whole grains, plant proteins, fatty fish full of omega-3s, and olive oil. It’s nutrient-dense, high in fiber and supports a healthy gut microbiome, which may contribute to better moods and better cognition.
The Mediterranean diet also avoids the health pitfalls that can come with a standard Western diet which tends to be full of sugary drinks, ultra-processed foods, and high-cholesterol meats. Science tells us that following a Mediterranean eating plan is linked to a lower depression risk, lower heart attack and stroke risk, and lower breast cancer risk, especially for postmenopausal women.
While the traditional Mediterranean diet slows age-related brain shrinkage, the Green Mediterranean diet amplifies those effects by adding anti-inflammatory green tea, avocados and soybeans.
Omega-3 + Vitamin D3 & K2 Supplement Support
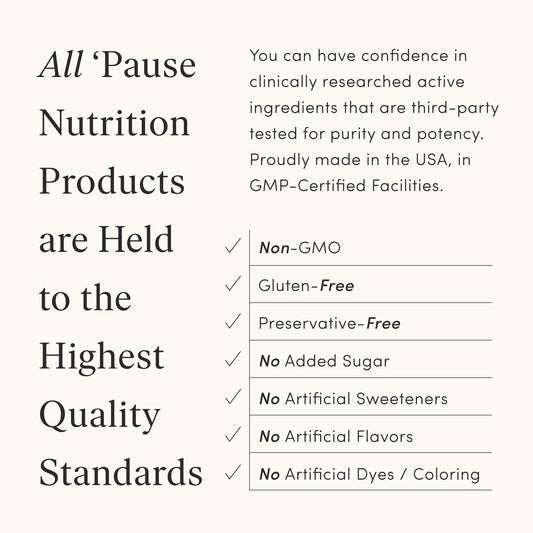
In addition to eating well, taking an omega-3 fatty acid supplement that also includes vitamin D3 and K2 may help to ease depressive symptoms, benefit emotional and cognitive behaviors, and lower inflammation in menopause.* Fiber is another important piece of the puzzle. If you’re falling short on the recommended 25 to 35 grams of fiber daily, a supplement like The Pause Nutrition Fiber GDX can be an easy way to catch up.*
Beyond nutrition, consistent habits and rituals matter. Practicing anti-inflammatory nutrition may mitigate some of the changes in the brain. Adequate sleep, routine exercise and practicing mindfulness may also help to decrease inflammation and cortisol. Together, they create a healthier brain environment during menopause and beyond.
The Bottom Line
Menopause brain fog is often temporary, but that doesn’t make it any less real. Whether or not you choose hormone therapy, building healthy lifestyle habits like nutrient-rich eating, exercise, stress reduction, and restorative sleep, can strengthen and support a healthy brain and body for years to come.