Endometriosis & Menopause: What You Need To Know

Share
For most women with endometriosis, menopause may feel like something of a blessing. Going through this transition can cause symptoms such as pelvic pain and heavy bleeding to become less severe or go away altogether. That's true for 96 percent of women, according to a menopause guide1 by The Endometriosis Network Canada.
However, two to five women out of 1002 will continue to struggle with endometriosis. Managing endometriosis can be complex, and that’s especially true after menopause.
What is endometriosis?
Endometriosis is a systemic inflammatory disease characterized at surgery by the presence of endometrium-like tissue found outside the uterus. It’s estimated that 10 to 15 percent3 of people born female develop endometriosis, and it’s much worse than heavy or painful periods. It’s a chronic inflammatory full body disease that can cause pain, gastrointestinal and other organ dysfunctions, infertility and other complications.
What causes endometriosis?
Researchers still aren’t certain what causes endometriosis, but there are many theories. Some theories suggest that one is born with endometriosis and combined number of factors trigger the disease, immunologic dysfunction and genetics just to name a few.
Some studies show that starting menstruation early4 can influence endometriosis risk, but other studies don’t bear that out.5 Heredity however, does play a role. If a woman has endometriosis, it’s five to seven times more likely6 that her sisters and children will too.
How is endometriosis diagnosed?
Given that 70 percent of women with chronic pelvic pain have endometriosis7, one might think it would be diagnosed more often. But, as with a variety of other conditions related to women’s health, many clinicians aren’t well informed8. The same 2021 study from DeMontfort University noted that endometriosis is called the ‘missed disease’9 because it has fallen into the chasm of willful ignorance about women’s bodies, dismissal of women’s pain10 and undone science due to the vast lack of government funding for research. Just 0.038 percent11 of the National Institutes of Health’s 2022 budget was devoted to endometriosis research, though it affects 6.5 million women in the US and more than 190 million worldwide.
Women can also have a range of symptoms, and for decades there has been no definitive blood test12 available to diagnose endometriosis, but that may be changing. A 2025 paper by Proteomics International in Australia identified a set of 10 blood protein markers13 that researchers believe will reliably diagnose endometriosis. Currently, the only way to diagnose the condition is with a laparoscopic excision surgical procedure. In the meantime, a 2023 study reminded clinicians to consider endometriosis whenever they see a patient with complaints of painful sex, chronic pelvic pain or severely painful periods.14
A 2007 study found most women spend eight to 12 years looking for answers15 and go to a general practitioner at least six times before a clinician comes up with a diagnosis. Treatments range from prescribing painkillers to progestin birth control to minimize periods to surgery to remove endometrial tissue or the uterus. Other women are put on medication to cause an early menopause.
Many others, an estimated 60 percent, never get a diagnosis that explains what’s happening. And 74 percent get the wrong diagnosis16 and ineffective treatment. Painful sex, infertility, bleeding in between periods, painful elimination and back pain that endometriosis causes often get attributed to other conditions including:
- Interstitial cystitis
- Urinary tract infections
- Irritable bowel syndrome
- Colitis
- Pelvic inflammatory disease
- Uterine fibroids
- Ovarian cysts
On arecent episode of her You Are Not Broken podcast, Dr. Kelly Casperson, a board-certified urologist in Bellingham, Washington, discussed endometriosis with Dr. Thaïs Aliabadi and Mary Alice Haney of SheMD. Dr. Casperson shared that she often sees women who likely have endometriosis who are referred for interstitial cystitis. They’ll have recurrent UTIs or tender pelvic floor muscles, both of which indicate that interstitial cystitis isn’t the cause. “I'm like, you actually listen to a woman, do a proper physical exam,” says Casperson to narrow down the diagnosis. “I take more interstitial cystitis diagnoses away from women.”
How does menopause affect endometriosis?
So it’s possible for a woman to reach menopause without knowing she has endometriosis. That’s concerning since women with endometriosis are at higher risk for some serious health conditions. One study found women with endometriosis are hospitalized for cardiovascular disease more often17 than women of the same age without endometriosis. As estrogen levels decline during menopause, that brings additional cardiovascular risks.
Obesity is also linked to a recurrence of endometriosis in postmenopausal women. The pain and challenges this condition brings means women with endometriosis are more likely to experience a brain health condition18 such as anxiety or depression.
Can Women with Endometriosis Use Menopause Hormone Therapy?
One of the most common misconceptions I hear from patients—and even some clinicians—is that women with a history of endometriosis are not candidates for menopause hormone therapy (MHT). The fear is that estrogen will “reactivate” dormant endometriosis implants and bring symptoms roaring back. And while there are some isolated case reports suggesting this is possible, the overwhelming consensus among menopause specialists is that this risk is extremely rare—especially when hormone therapy is carefully managed.
In our clinic, we regularly prescribe low-dose estrogen-based MHT to patients with a history of endometriosis. But here’s the key: we always pair it with higher doses of progesterone, regardless of whether the patient has a uterus. This helps keep any residual endometrial tissue from becoming hormonally active again. We also monitor symptoms closely and make adjustments as needed. It's a thoughtful, evidence-based approach—and it works.
Unfortunately, many women have been told—or have assumed—that hormone therapy simply isn’t safe for them because of their endometriosis history. But this blanket avoidance denies them the many benefits of MHT, including symptom relief and long-term protection for the brain, bones, and cardiovascular system.
Some clinicians may recommend more aggressive treatments, such as inducing early menopause with medication or removing endometriosis lesions surgically, even a hysterectomy. But here’s what’s often overlooked: if you remove the ovaries or suppress natural estrogen production, you still need to replace what’s been lost. Estrogen plays a critical role in maintaining whole-body health. Removing it without replacing it creates a new set of problems.
A 2023 study published in the Scandinavian Journal of Obstetrics and Gynecology stated clearly: “Menopausal hormone therapy (MHT) is the most effective treatment for menopausal symptoms.” And while endometriosis is fueled by estrogen, what often causes problems isn’t the presence of estrogen itself—it’s the fluctuations. Hormone therapy provides a steady, low dose of estrogen that avoids the hormonal rollercoaster.
As my colleague Dr. Heather Hirsch has explained so well in this YouTube video, this stability makes all the difference. And again—progesterone must be part of the equation.
Bottom line: if you’ve had endometriosis, you’re not automatically excluded from MHT. But you do need a provider who understands how to personalize your care, weigh your risks and benefits, and craft a regimen that works with your history—not against it.
How women with endometriosis can thrive during menopause
Endometriosis is a challenging condition but fortunately there; a growing awareness among women, clinicians and researchers. Here are some lifestyle habits to consider:
- Prioritize healthy weight. Just like for all menopausal women, maintaining a healthy weight is one of the best ways to nurture your body and your overall health.
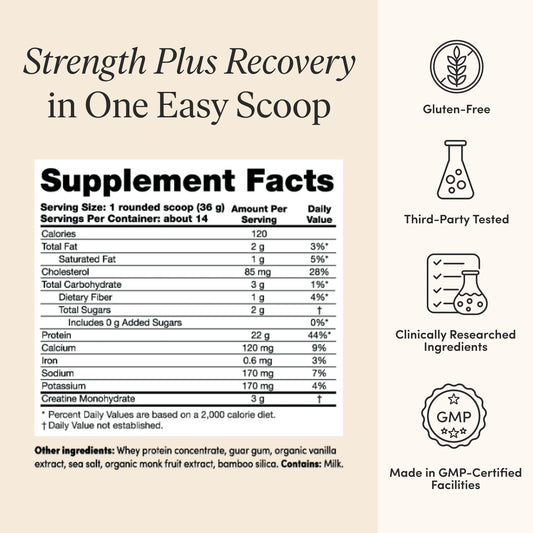
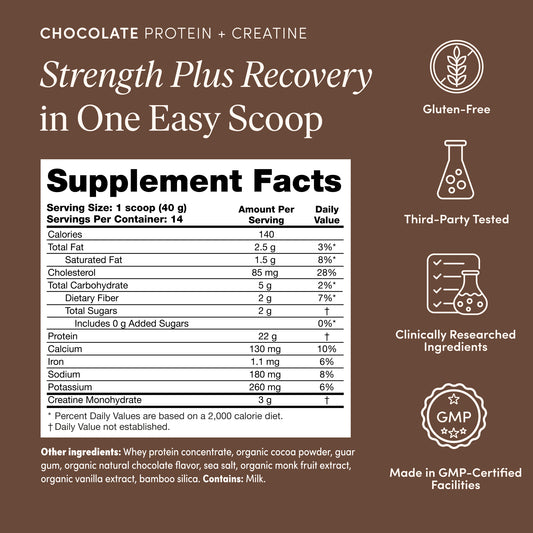
- Eat adequate protein. (here’s how to calculate how much you need) Consuming enough protein is one of the best ways to curb cravings and support building muscle. Find out how much you need with our Protein Calculator and track your intake with a nutritional tracking app such as Cronometer.
- Stay active. When you’re not feeling well, it's natural to seek the solace of a favorite armchair. But did you know regular physical activity has a wealth of benefits? Muscle is the organ of longevity and helps you keep blood sugar stable and bones strong. Researchers found exercise can be a very effective treatment for major depression.19 Walking, jogging, yoga and strength training are especially effective.
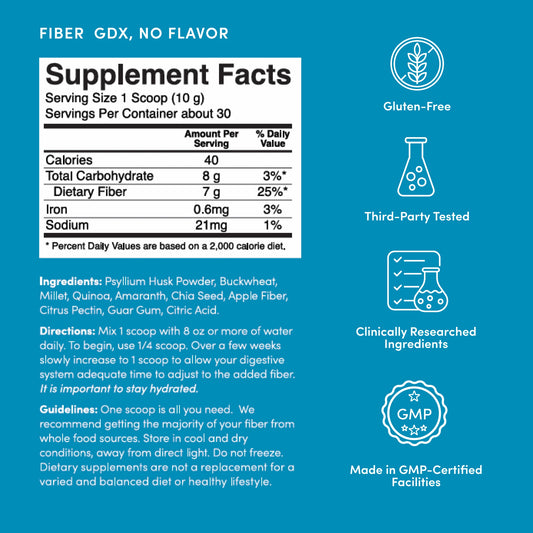
- Nurture your gut. The more researchers uncover about the gut microbiome, the more we learn how fundamental it is to every aspect of our health. And that includes endometriosis: women with the condition are more likely to have less diverse gut flora20 and more negative bacteria. Researchers believe that making sure the gut is healthy and populated with beneficial flora can help lower inflammation and reduce gastrointestinal symptoms like diarrhea nausea, bloating and constipation. Eating enough fiber and lots of colorful produce such as kiwi fruit and pomegranates will help keep beneficial gut flora happy, while lactobacillus probiotics21 have shown promise in reducing pain.
- Consider hormone replacement therapy. Each woman’s biology is different, so it’s important for each woman to evaluate the risks and benefits of hormone replacement therapy, and all the available options with a menopause-informed clinician.
Making these lifestyle shifts and keeping yourself (and your doctor) up to date on advancements in care may help you feel better and thrive at any age. For more information about endometriosis, visit The Endometriosis Summit website and consider attending an event, or The Center for Endometriosis Care.
For information on how to speak with your doctor, download my Menopause Empowerment Guide.