3 Ways Menopause Changes the Gut Microbiome

Share
3 Ways Menopause Changes the Gut Microbiome + 3 Natural Solutions
At first blush, it might seem like menopausal hormone changes would have nothing to do with our gut microbiome, trillions of microorganisms that line our entire digestive tract. But as we've been learning, nearly every body system has estrogen receptors and works better with sufficient estrogen. Our gut microbiome isn't any different.
While our gut flora makes enzymes that help break down the food we eat, it also assists in absorbing nutrients and vitamins. When gut flora ingests food with fiber, it produces needed nutrients like short-chain fatty acids (SCFAs). Our gut flora also makes more than 90% of our serotonin(1), an important neurotransmitter that helps regulate our digestion and mood. But the gut flora also does so much more.
Researchers now know that a whole contingent of gut flora dubbed the estrobolome(2), is dedicated to managing estrogen in the body. The estrobolome works to move estrogen around the body and to metabolize or break down estrogen so our hormone levels stay in the optimal range for health. Not only that, another squad of gut flora is also communicating with our brain via a network of nerves called the gut-brain axis(3).
In a healthy gut, the majority of the flora are beneficial and run things, releasing positive signals to our brain and body while keeping a few troublesome flora in check. Maintaining that needed balance becomes more challenging once our estrogen levels fluctuate and decline. If the bad bacteria start to take over, it can have negative effects on our mood, anxiety level, weight, metabolism, and overall health.
What changes in the gut microbiome after menopause?
As estrogen levels decline, the makeup of our gut flora changes. If things get too out of balance and harmful bacteria take over, we get into gut dysbiosis. Over time, this gut imbalance can lead to disease. Scientists are exploring how having a gut that's out of balance affects risk for conditions like cancer(4) and polycystic ovary syndrome(5) (PCOS).
Here are some specific changes that can happen after menopause.
Less microbiome diversity
Premenopausal women have a robust gut microbiome with many different gut flora—our gut diversity peaks around age 40. (6) After menopause, it starts to decline, and women's gut population begins to look more like that of men. A more diverse gut microbiome is beneficial because it helps better protect against germs and bacteria that can cause disease. In a 2023 study, researchers at the University of Oxford found that the more kinds of good flora(7) you have, the quicker they can shut down invading bacteria. The team at Oxford looked at how gut flora handled Salmonella enterica and Klebsiella pneumoniae. These two nasty pathogens can cause pneumonia, urinary tract infections, blood infections or gastroenteritis, and severe dehydration. They found that working alone, good gut flora couldn't do much to stop these pathogens. However, a community that included up to 50 kinds of good bacteria made these invaders grow 1,000 times more slowly.
Fewer beneficial gut bacteria
Most of us have a mix of many kinds of flora in our gut microbiome. While determining exactly what each type of gut flora does is still an emerging science, scientists know some are less beneficial, especially when we have too many. Postmenopausal women tend to have more strains that studies have linked to obesity, such as Dorea(8), Prevotella, and Sutterella, according to a 2022 review(9). When we have an overgrowth of specific flora, they can wreak havoc by releasing toxins that can lower our mood(10) or make us crave fat and sugar.(11) The same review noted that menopausal women have lower amounts of Ruminococcus, which makes short-chain fatty acids beneficial. They also noticed a dip in the level of Firmicutes, which can aid in getting nutrients, regulating hunger, and feeling satisfied.
Higher risk of health conditions, including depression and anxiety
Researchers found gut flora changes can explain why some women find themselves struggling with anxiety and depression during perimenopause and menopause. Older women are more likely to take antidepressants(12) than any other segment of the US population. Chinese researchers found that premenopausal women with depression(13) had 14 times more Klebsiella aerogenes, a gut flora that rapidly breaks down estradiol and clears it from the body. This left these women with 43% less estradiol than women who were not depressed. In another study, researchers found that women with perimenopausal panic disorder(14) had an imbalance of Bacteroides and Alistipes. While both of these can be beneficial, the overabundance causes the problem.
What can I do to improve my gut health?
There's a lot you can do to keep your gut healthy. Like so many other facets of health, it all begins with what you eat, supported by some special foods and a couple of effective supplements that keep the gut microbiota happy.
Eat colorful veggies and fruit full of fiber and nutrients
The number one thing you can do to support a happy, healthy gut with diverse flora is to eat an anti-inflammatory diet full of fish, whole grains, nuts, and colorful fruits and vegetables packed with fiber and nutrients. Studies show this Mediterranean way of eating is linked to improved gut health,(15) a more diverse gut microbiome, and more positive flora. Eating more plants will help lower inflammation(10), which is crucial whether I'm counseling patients who want to lose belly fat, reduce joint pain, or regain their libido. Equally important is avoiding foods that cause inflammation and can damage the microbiome, like highly processed foods, seed oils, artificial sweeteners, excess sugar, lots of meat, and, for some of us, wheat flour and dairy.
Boost gut health with probiotics, prebiotics, and synbiotics
If you've started exploring gut health, you've come across these terms: probiotic, prebiotic, and synbiotic(16). They all work together to support gut health.
A probiotic is a good bacteria that helps strengthen the positive flora you already have in your gut. There are many different families of probiotic bacteria, and they can help with other aspects of gut health. For example, akkermansia muciniphila(17) is considered a star probiotic bacteria that can support immune health and lessen the risk of metabolic conditions. Other popular probiotics include strains of lactobacillus(18) and bifidobactcterium(19), which support immune function. You can take probiotics in capsule form, but one of the easiest ways to get them is by eating probiotic foods such as fermented vegetables and dairy foods such as sauerkraut, kimchi, miso, yogurt, and kefir.
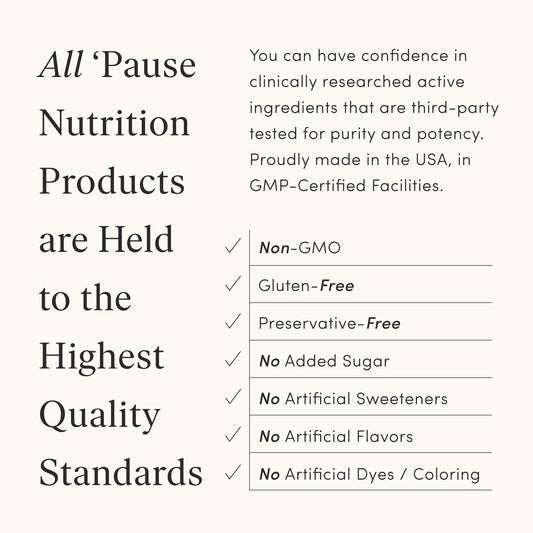
Prebiotics are non-digestible plant fibers that our beneficial gut bacteria eat to stay healthy. Many plant foods, including kiwi fruit, pomegranate, flax seeds, onions, and bananas, are considered prebiotic. If you're getting the recommended 25 to 35 grams of fiber per day from black beans, purple cabbage, chia seeds, and avocados, you're probably getting the prebiotics your body needs. The suggested daily intake for prebiotic fiber is 3 to 5 grams. I recommend you get most of your fiber through whole foods, but should you fall short, consider adding a supplement with soluble and insoluble fiber like The 'Pause Nutrition Fiber GDX.
Synbiotics are a newer approach to improving gut health, containing a probiotic-prebiotic combo that works in synergy. There are some foods considered synbiotics, such as miso soup made with fermented miso paste and soybean fiber or yogurt mixed with flaxseed or pomegranate arils. However, a synbiotic is usually a supplement that pairs beneficial gut flora strains with the particular fiber that those strains need to grow. Synbiotics are considered a more practical approach to boosting gut health, and one of my favorite choices is the Alloy Synbiotic. Made with golden kiwi fruit prebiotic fiber and citrus flavonoids, Alloy Synbiotic's specially selected probiotics can help you build a healthy gut microbiome to support better immune function and overall health.
Consider menopausal hormone therapy
In a small 2022 study, researchers compared the upper small intestines of premenopausal women, menopausal women on hormone therapy, and menopausal women not taking hormones. They found that the women on hormones had more diverse gut flora(20) and a similar mix as premenopausal women. These groups had more Prevotella (a positive in this study) and fewer Escherichia and Klebsiella. Women without hormone therapy had more proteobacteria (a strain linked to metabolic conditions and bowel inflammation), fewer Bacteroidetes, and lower gut diversity overall.
Perhaps now, you have a better understanding of how to support your gut flora. For a happy and healthy gut, eat more veggies and fiber and consider adding a gut supplement to your routine. All of that is good for you! However, don't worry if you experience some bloating or gas for the first couple of weeks. Remember, your old gut flora that liked a diet of burgers, fries, and sweet coffee drinks may become cranky when you switch to eating kale Caesar salads and chia pudding!
If discomfort lasts more than a couple of weeks, check with your clinician to ensure you're not dealing with a more serious condition like small intestinal bacterial overgrowth. Slowly but surely, you'll see your body adjust, and soon, you'll be craving all those fiber-rich whole grains, fruits, and veggies. Really!
This article contains affiliate links.