Misdiagnosis in Perimenopause: Understanding Overlooked Common Conditions

Share
Perimenopause is a transitional phase in a woman’s life, marked by fluctuating hormones and unpredictable changes in her body. Unfortunately, the lack of education and awareness about perimenopause among healthcare providers has led to a dramatic increase in misdiagnosed conditions during this time. Many women experiencing the onset of perimenopausal symptoms are instead diagnosed with conditions such as ADHD, leaky gut syndrome, fibromyalgia, long COVID, interstitial cystitis, adrenal fatigue, depression, anxiety, or even fatty liver disease.
These conditions are legitimate diagnosis, but when they appear in perimenopausal women, they may, in fact, be misattributed manifestations of the hormonal shifts occurring during this phase. This is often due to a lack of formal menopause training in medical schools and residencies, leaving frustrated clinicians to rely on vague or exclusionary diagnoses to help their patients.
Let’s dig deeper into some of the most commonly misdiagnosed conditions.
ADHD: Perimenopause or Misdiagnosed Cognitive Decline?
A surprising diagnosis often given to perimenopausal women is attention-deficit hyperactivity disorder (ADHD). Women in midlife may report difficulty focusing, poor memory, and general cognitive decline—symptoms that overlap significantly with those of ADHD. However, this mental fog is often a result of hormonal fluctuations during perimenopause, particularly declining estrogen levels, which affect neurotransmitters in the brain like serotonin and dopamine. (1) These shifts can impair memory, focus, and cognitive sharpness. Many women who are incorrectly diagnosed with ADHD during perimenopause may instead be experiencing what is sometimes referred to as “menopause brain.” The lack of proper menopause education among clinicians may lead to an unnecessary ADHD diagnosis when perimenopausal hormone changes are the underlying cause. (2)
Leaky Gut and Fibromyalgia: The Elusive Diagnosis of Exclusion
Conditions like leaky gut syndrome and fibromyalgia are frequently diagnosed in perimenopausal women, often as “catch-all” diagnoses when no clear explanation is found for their symptoms.
Fibromyalgia, in particular, is a diagnosis of exclusion, meaning that when other conditions are ruled out, this label is given to explain widespread pain and fatigue. Yet many of these symptoms, including joint pain, muscle aches, and exhaustion, are well-documented signs of hormonal changes during perimenopause. (3)(4)
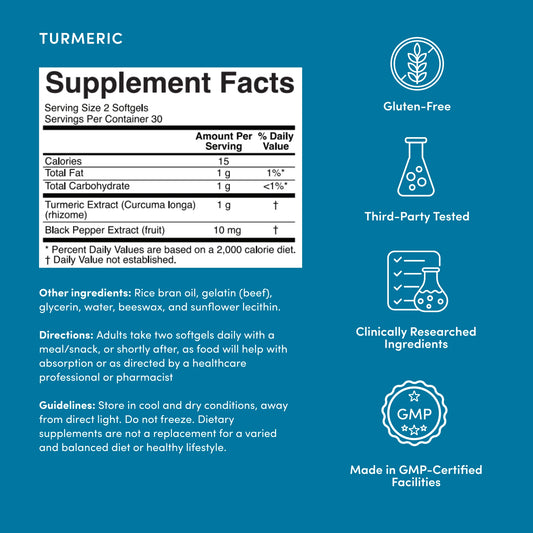
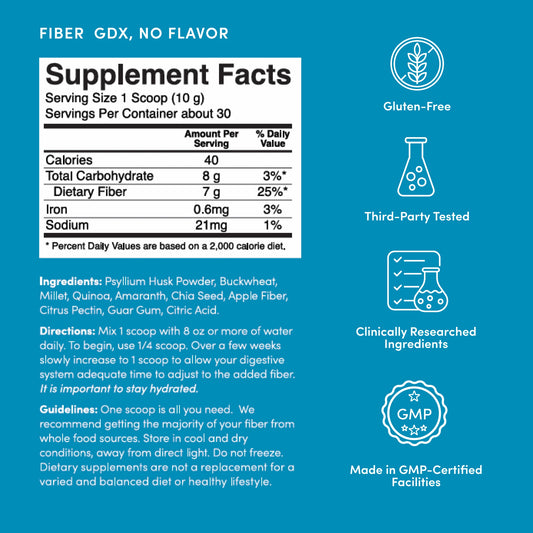
Similarly, leaky gut syndrome, which is often used to explain digestive discomfort, may be triggered by changing hormone levels affecting gut function. (5)(6) Nourish the beneficial gut bacteria, strengthen the gut barrier, and support normal inflammatory levels with fiber rich foods and a fiber, probiotic or synbiotic supplement.*
While both fibromyalgia and leaky gut are real conditions, their increased prevalence in perimenopausal women suggests that hormonal fluctuations are often the real culprit, and not necessarily these more elusive diagnosis.
Long COVID and Interstitial Cystitis: Misdiagnoses or Menopause Manifestations?
Long COVID, a relatively new diagnosis resulting from the ongoing pandemic, has a striking overlap with perimenopausal symptoms. Fatigue, brain fog, and muscle pain are some of the key features of long COVID, but these are also hallmark signs of the menopause transition. (7)
Similarly, interstitial cystitis, an often painful and frustrating bladder condition diagnosed in many perimenopausal women, may sometimes be incorrectly attributed to chronic pelvic pain that is instead driven by falling estrogen levels, which influence bladder health. (8)
This overlap in symptoms can result in misdiagnosis, leading women to seek treatments for conditions that are in fact manifestations of perimenopause.
Adrenal Fatigue and Mental Health: Are They Really Hormonal Shifts?
"Adrenal fatigue," is another diagnosis commonly given to perimenopausal women reporting extreme fatigue and poor stress tolerance. Many women are told their adrenal glands are underperforming, but this diagnosis is not well-supported by evidence in conventional medicine.
In fact, declining estrogen during perimenopause can explain much of this fatigue, as estrogen plays a key role in energy metabolism and mood regulation. Similarly, depression and anxiety are frequent diagnoses given to women during this phase, but much of this emotional distress is tied to hormonal fluctuations rather than a psychiatric disorder. (9)
Perimenopausal women often describe feelings of despair, mood swings, and heightened anxiety, yet these symptoms are part of the normal transition through menopause. (10)(11) Without proper training, clinicians may default to antidepressants or anti-anxiety medications instead of addressing the underlying hormonal imbalance. (12) Consider adding meditation or other aids to further support your mental health.
Fatty Liver: A Metabolic Consequence of Perimenopause
Another condition on the rise in perimenopausal women is non-alcoholic fatty liver disease (NAFLD), which is increasingly being linked to the metabolic changes that occur during this transitional phase. (12)
Estrogen plays a protective role in regulating liver metabolism, and its decline can lead to an increase in fat storage in the liver. Women may be diagnosed with fatty liver disease when, in fact, the cause may be the metabolic syndrome of menopause.
Many clinicians are unaware of the role estrogen plays in liver health, leading to confusion and an inaccurate diagnosis when perimenopause is the root cause. (13)
The Lack of Education and Awareness: A Systemic Issue
These misdiagnoses highlight a systemic issue in the medical community: a lack of education and awareness about menopause and its effects on the female body. Many of these diagnoses are not wrong per se, but they are often applied without considering the role of perimenopause.
The fluctuating hormone levels during this phase, especially estrogen, progesterone, and testosterone, affect nearly every organ system, from the brain and digestive tract to the muscles and liver. Yet, few medical professionals are trained to recognize these hormonal influences, leading to vague diagnoses born out of frustration.
Clinicians often want to help their patients, but without the proper tools or understanding, they fall back on exclusionary diagnoses or well-meaning but incomplete labels.
Conclusion: The Need for Improved Menopause Education
The dramatic rise in diagnoses such as ADHD, leaky gut, fibromyalgia, long COVID, interstitial cystitis, adrenal fatigue, depression, anxiety, and fatty liver in perimenopausal women may often reflect the effects of perimenopause itself rather than separate, unrelated conditions.
The lack of formal menopause education in medical training has left many clinicians ill-equipped to diagnose and treat women in this stage of life properly. As a result, women may be receiving treatments for conditions that are actually manifestations of the menopause transition.
Addressing this gap requires comprehensive training in menopause and hormone health, ensuring that perimenopausal women receive accurate diagnoses and appropriate care tailored to their specific needs.
Download The ‘Pause Life Menopause Empowerment Guide for more information, resources and tips on how to advocate for yourself and the care you deserve.

This article contains affiliate links.