The Black Menopause Experience

Share
By Maria C. Hunt
When Dr. Jayne Morgan was in her 40s, she says she started noticing some strange and annoying symptoms. First her ears started itching. As she was teaching one of her Pilates classes, she felt dizzy, which had never happened before. And then her heart started racing out of nowhere.
“Itchy ears, vertigo and palpitations: those are symptoms I wasn’t really attributing to perimenopause at all,” says Morgan, a cardiologist based in Atlanta. While menopausal Black women experience severe hot flashes which raises cardiovascular risk, it’s often subtle, seemingly unrelated changes that signal they’re entering this crucial transition. And these symptoms of declining estrogen are easy to miss since they often start earlier than for other women.
Morgan says her friends have complained about hair thinning and changes in hair texture. “I think we see a lot of things in our hair. My hair is so unmanageable. My conditioner doesn’t work anymore,” Morgan recalls. The problem may not be the conditioner. Some researchers believe estrogen deprivation can sendhair follicles into their own menopause.(1)
And when you do connect those little changes with menopause, Black women often don’t get help from healthcare teams. Even though Black women have more severe hot flashes, which start earlier and last longer, studies show they’re less likely to get menopausal medical treatment(2), referrals or medication. This creates a health inequity, says Dr. Jessica Shepherd, an OB/Gyn, who runs Sanctum Wellness in Dallas. “I think it falls into the lump of Black women are not being heard,” Shepherd says. “I’m expressing my complaint yet it’s not being addressed.”
“Black Women Are Not Being Heard”
The phenomenon isn’t unique to menopause care; whether they’re recovering from childbirth(3), undergoing cancer treatment or suffering with bone fractures(4) or backaches, Black women and men are less likely to get pain medication(5). And if they do, it’s a smaller quantity or lower strength(6), because of biased and erroneous beliefs they’ll become addicted. Studies show that a surprising number of medical residents and health providers incorrectly believe that Black people feel less pain than white people (7) – a vestige of enslavement when Black suffering was routinely ignored.
So, given this backdrop, as a menopausal Black woman, you need to be prepared to advocate for yourself like your life depends on it, because in many ways it does. “I don’t think there’s any group that needs to advocate for themselves more than Black women,” says Dr. Sharon Malone, Chief Medical Advisor of Alloy Women’s Health.
Malone, who was a practicing OB/gyn for 30+ years, says Black women may hold a cultural belief that gutting it through hot flashes shows strength. But severe and frequent hot flashes are a warning sign of cardiovascular distress. Studies show leaving severe hot flashes and night sweats untreated is associated with increased risk of dementia(8), heart disease(9) and stroke(10) in women who also get migraines. Since Black women tend to start menopause earlier, our heart disease risk starts earlier. Heart disease is the number one killer of Black women(11) and strokes are the third leading cause of death.
Our skin may still be free of wrinkles and fine lines, we need to look deeper
“[We say] Black don’t crack. That’s on the outside,” says Morgan, chief medical officer for Hello Heart, a digital company based in Northern California. “On the inside, we may have more advanced age than our counterparts.” That’s because of “weathering,” a hypothesis developed by public health researcher Arline T. Geronimous, PhD and detailed in the book of the same name. It explains why Black and other women of color can experience health declines earlier than white women of the same age. “It’s a result of high-effort coping in a race conscious and gener conscious society and the wear and tear it takes on our bodies,” Morgan says. “Over time, your biological age may be 10 years older.”
As estrogen levels fall during perimenopause and menopause, our arteries become more stiff, leading to high blood pressure, Morgan explains. Estrogen is generally anti-inflammatory, keeps our vasculature and our arteries in a more relaxed state. “So replacing that estrogen provides protection for the heart,” Morgan says. “I think HRT is excellent for many women. It’s not right for everyone. Every woman should have the right to have this conversation with their doctor about whether HRT is right for them.”
Focus on These Healthy Habits
Besides the basics like quitting smoking and limiting alcohol, Morgan and Malone recommend focusing on these healthy lifestyle habits:
Eat anti-inflammatory foods + adequate protein.
Follow a diet with sound nutrition based on anti-inflammatory foods, including colorful vegetables like sweet potatoes, purple cabbage, collard greens and black eyed peas. Be sure to get adequate protein from fatty fish, lean cuts of meat, beans and nuts, aiming for 30 grams per meal.
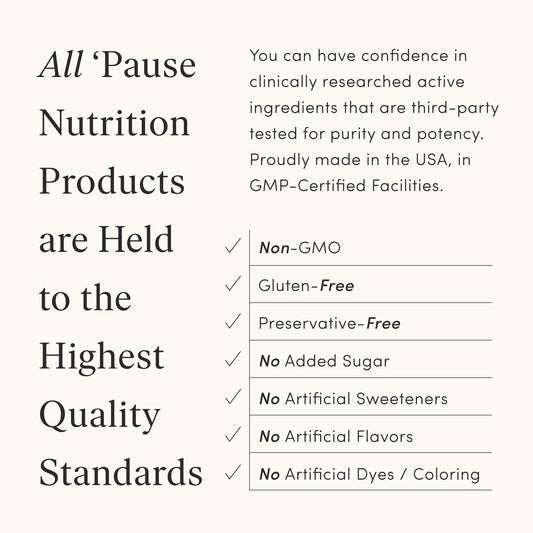
Avoid processed convenience foods with high sugars
If you’re a typical person living in the U.S., about 58% of what you eat is ultra processed foods. “We have an entire generation raised on processed foods,” says Malone. The additives, colors and sugars in these foods disrupt the microbiome,(12) which weakens our immune response. A diet high in processed foods is also linked to higher risk for cardiovascular disease(13), type 2 diabetes(14), breast(15), and colorectal cancer(16), which is rising rapidly in younger people. Going back to whole, natural foods like your Grandma ate is a powerful way to protect your health.
Move regularly
It’s important to fight muscle loss and bone thinning by doing resistance exercise regularly. If you don’t like lifting weights, try bands or Pilates, and keep your cardiovascular system fit with walking, running, pickleball or dancing; just find an exercise you like and will do regularly.
Protect your mental health
Given the daily stresses Black women face, Malone says it’s not surprising that in menopause, they have higher rates of depression,(17) irritability and anxiety compared to white women. Prioritizing mental health is a form of self-care, and she urged women to find a provider in person or online to find the support they need.
And if you are one of the rare Black women who has access to a menopause-trained clinician who prescribes hormone replacement therapy, Malone urges women to please follow through and take it. There’s research showing some Black women are distrustful based on old, debunked fears about hormone safety. “There is a lot of conversation amongst ourselves. We will talk ourselves out of it,” Malone says. “You get a friend and someone will say, girl, ‘why are you taking those hormones?’ What it amounts to is a lot of suffering.”
Here are some Instagram accounts to follow:
- Dr. Jayne Morgan @drjaynemorgan
- Dr. Jessica Shepherd @dallasgynecologist
- Dr Sharon Malone @smalonemd
- Omisade Burney Scott @omisadeburneyscott
Read:
- Grown Woman Talk by Dr. Sharon Malone
- Generation M: Living Well in Perimenopause and Menopause by Dr. Jessica Shepherd
Visit:
Studies to explore:
- Disparities in Reproductive Aging and Midlife Health between Black and White women: The Study of Women’s Health Across the Nation (SWAN)
- Hormonal activity in commonly used Black hair care products: evaluating hormone disruption as a plausible contribution to health disparities
- Black women's hair: the main scalp dermatoses and aesthetic practices in women of African ethnicity
- Changing trends in Black-White racial differences in surgical menopause: a population-based study
Maria C. Hunt is a California-based journalist and author specializing in cultural stories around cuisine, beverages, travel, and wellness, particularly menopause and ethnic health disparities.