Understanding DHEA for Genitourinary Syndrome of Menopause

Share
Estrogen is the gold standard and most common treatment for pain and discomfort experienced in the vulvar and vaginal area related to menopause. However, there is growing interest in the use of dehydroepiandrosterone (DHEA) therapy to help relieve menopause-related symptoms in the genital area. Let’s discuss.
Genitourinary syndrome - Pain “down there”
Genitourinary syndrome of menopause (GSM) is a condition causing uncomfortable, painful, or bothersome vaginal and urinary symptoms during and after menopause. Previously known as atrophic vaginitis or vulvovaginal atrophy, GSM is caused by declining estrogen that occurs with the menopause transition. The decrease in estrogen causes physical and functional changes to the vulva, vagina, bladder, and urethra. (1, 2) These physical changes include:
- Thinning of the vulva (the external parts of the female genitals, including labia and the opening of the vagina)
- Decreased skin elasticity and blood flow
- Decreased lubrication of the vagina and vulva
- Loss of pelvic floor strength and control
- Changes to vaginal pH
- Falling or slipping (prolapse) of pelvic organs, vaginal vault, or urethra from their usual position
- Decline in bladder capacity and sensation
- Hypersensitivity or decreased feeling in the vaginal area

Up to 15% of perimenopausal and 84% of postmenopausal women are affected by GSM, with symptoms routinely impacting their daily life. (2, 4) The most common symptoms include:
- Genital dryness, burning, and irritation
- Decreased lubrication and pain with sexual activity
- Change to vaginal discharge
- Urinary urgency
- Pain with urination
- Urinary incontinence or leaking
- Recurring urinary tract infections (UTIs)
Despite the high number of people impacted, many are hesitant to discuss this issue with their healthcare provider due to the sensitivity of the topic, embarrassment, or the assumption that their symptoms are a normal part of aging. The symptoms of GSM are chronic and often worsen if not treated, leading to a decreased quality of life for those affected.
GSM is an unfortunate - but common - condition during menopause, but treatments available. This does not have to be your “new normal”.
DHEA – An alternative to estrogen
Again, hormone therapy in the form of topical estrogen is the most common and effective treatment for women experiencing GSM symptoms. (10) Topical estrogen has fewer risks associated with use than oral estrogen and is generally considered safe. However, for those who choose not to use vaginal estrogen, Dehydroepiandrosterone (DHEA) is an alternative.
DHEA is an androgen hormone produced during the reproductive years, primarily by the ovaries and adrenal glands which are located one on top of each kidney. (5, 6) DHEA converts to both testosterone and estrogen, and after menopause, becomes the primary sex hormone. (2, 5, 10) Studies show taking DHEA may help relieve some of the discomfort associated with GSM.
How do I get DHEA?
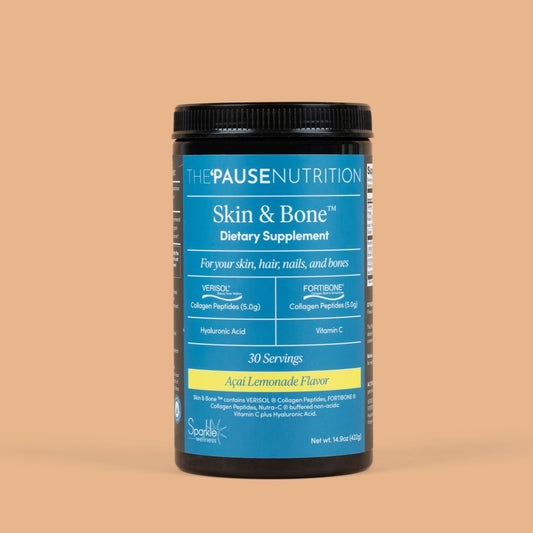
Oral forms of DHEA exist but there is no data proving it is effective in treating genitourinary symptoms and therefore, is not recommended. DHEA vaginal inserts are sold over the counter, but unlike prescription medications, dietary supplements are not regulated by the Food and Drug Administration (FDA) for safety and effectiveness. (8) For this reason, I suggest seeking out a brand that has been third-party tested.
Prasterone, a synthetic version of DHEA, is an FDA approved vaginal insert and can be prescribed by your healthcare provider. When placed nightly inside the vagina, the medication works to relieve pain from sexual activity related to drying and thinning of vulvar skin caused by menopause. Some people also experience improvement in vaginal lubrication and sexual arousal as well. (9)
The exact method of how the medication works is unknown, but it is believed to stimulate the metabolism of estrogens and androgens in the vulva. (9)
Is DHEA supplementation or prasterone safe?
Like all medications, there are potential risks and side effects to prasterone use. The most common side effect reported is increased vaginal discharge. Studies have not found that DHEA or prasterone suppositories increase the amount of hormones circulating in the blood.
The medication is not associated with the development of endometrial cancer and may be used in consultation with an oncologist for individuals with current or past history of breast cancer. (9) Anyone with abnormal and undiagnosed genital bleeding should not use DHEA or prasterone suppositories.
For those experiencing discomfort in the vulvar and vaginal areas related to GSM, relief of symptoms can improve quality of life and sexual enjoyment. DHEA and/or prasterone suppositories are a safe and effective treatment for the relief of vulvar and vaginal discomfort caused by the loss of estrogen in menopause.
If you have symptoms, please do not be afraid to discuss them with your healthcare provider. There are safe and efficacious treatment available and your clinician can help you find relief.
Download my Menopause Empowerment Guide for tips on how to approach your healthcare provider about this, or other bothersome symptoms you may be experiencing.