Uncommon Signs & Symptoms Of Perimenopause & Menopause

Share
Beyond Hot Flashes: Symptoms Of Perimenopause And Menopause That May Surprise You
We have all heard about hot flashes and night sweats, but there are many more symptoms that you may not realize are related to the menopause transition. Did you know that the fluctuating hormone levels associated with perimenopause and menopause can lead to musculoskeletal problems, changes in your sense of taste, and heart-rhythm irregularities?
Many of the challenges that come along with menopause are also symptoms of more serious medical conditions. If you are suffering from some of these problems, it is important to speak with your doctor to rule out other possibilities. Once you and your doctor feel that menopause is the culprit, you can work together to manage these symptoms and feel better.
Menstrual Changes
Having periods that are lighter or heavier, or occur more frequently or less frequently than usual, is the most common symptom of perimenopause. Menstrual changes are often the first sign of the menopause transition.
Vasomotor Symptoms
During perimenopause and menopause, declining estrogen levels cause hot flashes and night sweats which are examples of vasomotor symptoms (VMS).
Hot Flashes
Hot flashes are common during perimenopause and menopause. Most people experience hot flashes, which feel like heat/sweating/flushing in the head and upper body regions, during midlife.
Night Sweats
Hot flashes that happen while sleeping are called night sweats, which may cause people to wake up drenched in sweat and have a hard time falling back asleep. The 'Pause Life team has curated some of their favorite cooling products in 'Pause Favorites.
Weight Gain And Weight Redistribution
As estrogen levels drop, fat distribution begins to shift from the hips and thighs to the abdomen, in the form of visceral fat, which isn’t just unsightly, it’s also dangerous. During perimenopause and menopause, many experience this increase in visceral fat along with a decrease in muscle mass which studies have shown raises the risk of developing heart disease, diabetes, dementia, and certain cancers.
Psychological Changes
Hormone fluctuations can trigger several different types of psychological and mood changes. Those who have a history of depression or anxiety may have increased difficulty during the menopause transition. It is not uncommon to experience; depression, anxiety, irritability, mood swings or panic attacks.
Sleep Disturbances
Difficulty falling asleep or staying asleep are both common during the menopause transition. Some sleep disturbances can be attributed to waking up because of night sweats. Fragmented or poor-quality sleep is linked to weight gain and depression, which are other challenges many face during menopause.
Fatigue
Many people feel fatigued or exhausted during menopause. This can be caused by fluctuating hormone levels, sleep disturbances, or a combination of both. Fatigue can result in feeling tired both physically and mentally.
Sexual Dysfunction
Vaginal Changes
Decreased estrogen levels leave vaginal tissue feeling drier and less elastic. The tissue becomes thinner and may tear, causing pain during intercourse. In addition, vaginal secretions lessen which means less lubrication. Lubricants and vaginal moisturizers may ease discomfort and provide temporary relief, but please note that they will not rebuild the tissue or reverse atrophy.
Decreased Libido
Many people in perimenopause experience reduced sexual desire. This can be caused by a decrease in the level of estrogen and testosterone that was present earlier in life.
Tender Breasts
Sore or tender breasts are one of the early indicators of perimenopause. Changing levels of estrogen and progesterone lead to breast tenderness, similar to what happens during premenstrual syndrome. However, some report the tenderness feels differently during perimenopause. Burning and throbbing sensations may affect some in midlife, as opposed to a dull ache that may have been felt earlier. Once you reach menopause, breast tenderness usually subsides.
Gastrointestinal Problems
Digestive Issues
Estrogen and progesterone play a role in digestion. When the hormone levels decline, your body has less of what it needs to create bile and digest food. Problems like acid reflux, diarrhea, and constipation may result.
Bloating
In addition to digestion changes, menopause can be accompanied by water retention that leaves many feeling bloated.
Neurological Changes
Migraine Headaches
Hormone changes can trigger migraines. Some experience migraines at different times during their menstrual cycle because of the change in estrogen levels. During menopause, the hormone fluctuations are more dramatic and can set off painful migraine attacks that can include nausea and sensitivity to light and sound.
Brain Fog
Feeling unfocused and having difficult concentrating, often called “brain fog,” is a common complaint during menopause. Sometimes brain fog is caused by the sleep disturbances or fatigue that can come with decreasing hormone levels.
Memory Problems
Estrogen supports memory function, so when it begins to decline, you may feel like you are less able to recall names and other facts.
Dizziness
Estrogen and progesterone affect inner-ear function. When the inner ears do not function at their full capacity, you may feel dizzy. Another cause of dizziness is dehydration which can happen from prolonged hot flashes or night sweats.
Tingling Or Shock-Like Feelings In Arms, Hands, Legs, Or Feet
Estrogen also plays a role in the central nervous system. Declining levels can cause intermittent discomfort in the extremities. This can feel like a tingling sensation under the skin, or you may experience what feels like a mild electrical shock. These sensations are harmless but can be aggravating.
Musculoskeletal Problems
Joint Pain And Muscle Aches
Many people in perimenopause suffer from widespread body aches, muscle aches, and joint pain. Pain in the feet, knees, shoulders, elbows, and hands are common during menopause. Estrogen helps to reduce the body’s inflammation, and when it declines, joints have less of the natural lubrication that helps them move easily and without pain. Many report suffering from menopause-related arthritis.
Osteoporosis
Estrogen supports bone strength. Without enough estrogen, bones may become weak or brittle, and your risk of osteoporosis increases. Those in menopause need to be alert and aware of their surroundings to help prevent unexpected bone fractures.
Heart Palpitations
The feeling that your heart is racing, pounding, or fluttering is a sign of heart palpitations. Typical episodes that occur during menopause are usually short lived and harmless. When estrogen levels decline, your heart can become overstimulated which leads to an increased heart rate and frequency of palpitations. Irregular heartbeats that happen frequently or increase in frequency could be a sign of another cardiovascular condition and should be evaluated by a healthcare provider.
Changes In Skin, Nails, And Hair
Dry, Itchy Skin
Decreased elasticity in the skin is one of the effects of declining estrogen levels during menopause. With less estrogen, skin is less able to retain the water it needs to stay hydrated. This means your skin may feel overly dry. You may also notice your skin is more sensitive than usual and may become irritated or itchy. Many experience unexplained rashes during menopause.
Weak Or Brittle Nails
Less moisture also affects fingernails and toenails. This can leave your nails feeling weak and brittle, and they may break or tear easily.
Hair Loss
Decreases in the amount of estrogen produced by the ovaries can cause hair loss or thinning hair.
Dry Or Itchy Eyes
Chronic itchy, scratchy, or dry eyes can be caused by reduced estrogen production. This can affect your body’s ability to create tears and may lead to blurred vision, swollen eyelids, or light sensitivity.
Burning Sensation In The Mouth
Burning mouth syndrome can occur during menopause. This condition produces burning, tingling, hot, or numb sensations in the mouth even though there is no injury or illness in the mouth. The area around the tip of the tongue is most frequently affected. People may also experience dry mouth.
Taste Changes
Less moisture in the body affects saliva production. In addition to burning sensations or dry mouth, some experience changes in how food tastes during menopause. A metallic taste in the mouth may occur.
Urinary Dysfunction
Declining hormone levels can weaken the muscles in the pelvic floor. These muscles control bladder function. The result can be urinary incontinence and some may release urine without warning. Many may also suffer from overactive bladder (OAB) which causes the sudden, frequent urge to urinate.
Allergies
There is a connection between hormone levels and the release of histamine in your body. Histamine causes allergy symptoms like sneezing, runny nose, and congestion. Some experience new or increased allergy symptoms during menopause.
Body Odor
Increased perspiration during hot flashes or night sweats can lead to body odor. Hormone fluctuations are also linked to an increase in the production of odor-causing bacteria. Dr. Shannon Klingman, obstetrician-gynecologist and the founder and inventor of Lume Deodorant, developed the aluminum-free deodorant line to address odor on the underarms and other parts of the body.
How To Manage Menopause Symptoms
Once you have begun the menopause transition, you may feel overwhelmed by bothersome symptoms. Many of these symptoms can be controlled or improved by making some lifestyle changes, and you can have a better quality of life.
I give my patients a Menopause Toolkit with 6 key strategies to reduce menopausal symptoms by creating habits that reduce inflammation. This toolkit is not a magic pill, but rather six strategies to incorporate into your lifestyle to enhance well-being and counteract menopausal symptoms.
-
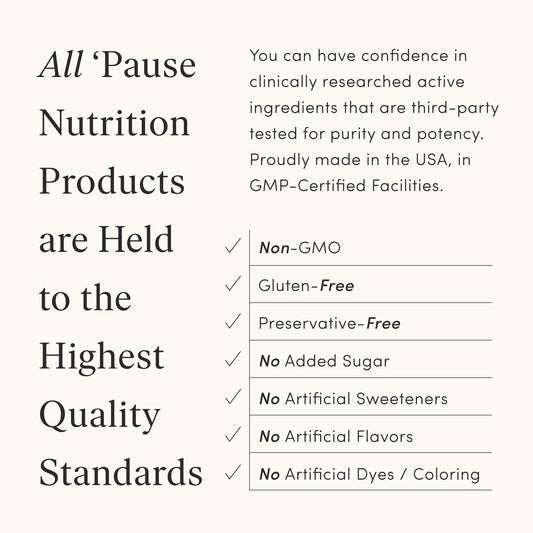
Nutrition: An anti-inflammatory approach to food reduces many symptoms of menopause like weight gain, bone loss, and the risk of chronic diseases such as heart disease and diabetes. An anti-inflammatory lifestyle, like what's outlined in The Pause Strong Program, focuses on lean meats, a variety of fruits and vegetables, whole grains and healthy fats. Increasing your intake of fiber and other vitamins and minerals, considering supplementation to fill in any nutritional gaps, and reducing your consumption of added sugars are foundational - but powerful - lifestyle changes that can improve your quality of life by leaps and bounds.
I wrote The Pause Strong Program to provide you with the information you need to develop more confidence in your nutritional choices. With some small, intentional changes, you can start creating a happier and healthier lifestyle.
-
Exercise: In addition to an anti-inflammatory diet, it is essential to incorporate resistance training and aerobic exercise on a regular basis to build strong muscles, bones, and bodies. Resistance training with weights, body weight or bands can help strengthen muscles and bones, and aerobic exercise, such as brisk walking, jogging, and running can help build bone density and maintain cardiovascular health. I have some great fitness equipment recommendations in 'Pause Favorites. The bottom line: Move your body. Exercise to be strong, not skinny.
-
Pharmacology: Discuss possible treatments with your healthcare provider to reduce symptoms such as hot flashes, night sweats, bone loss, premature estrogen deficiency, and genitourinary issues like vaginal dryness and frequent urination.
Hormone Therapy (HT) has been approved by the FDA to treat conditions related to menopause, and for many, this is a great option. For those who may not be good candidates for hormone therapy, there are other medications and supplements available that can be very effective in treating your symptoms.
It is important to meet with your provider to review your wants, needs and family history, so that together, you can determine what methods and treatments are the best fit.
-
Stress Reduction: Stress reduction techniques can reduce many symptoms, cortisol levels and some of the discomfort related to menopause. Practicing mindfulness, meditation and breathing techniques can help reduce many symptoms related to menopause and can lower acute stress and cortisol levels over time. The Waking Up app or Happier Meditation are great for guided meditations, or you may even consider scheduling some time with a counselor or therapist.
-
Sleep: The quality of your sleep is an essential component of your menopause toolbox. Without 7 to 8 hours of sleep a night, cortisol levels increase and cause inflammation in the body potentially leading to lowered defenses in the immune system and an increased risk of developing many chronic conditions such as sleep apnea and insomnia. It’s important to make time and create a bedtime routine that can help you get restful sleep.
-
Community: Being part of a community enables you learn from others and provide encouragement and accountability, while enjoying a sense of togetherness, commonality and belonging.
I invite you to join our FREE The ‘Pause Life Community! Form connections to help you build your confidence and reach your goals. There’s truly nothing like belonging to a community of like-minded people to keep you focused, celebrate your wins, commiserate your struggles and lift you up when you need it most!
As with anything else, you will get out what you put in, so be an active participant in whatever community you choose to be a part of.
The six strategies in my Menopause Toolkit outlined above support one another and produce a plan of action to help manage symptoms of perimenopause and menopause. With some small changes like the ones outlined in the Menopause Toolkit, you can literally improve your health, feel vibrant, energetic and excited about this stage of your life!